“Patients are sitting on a treasure trove of data about their own medical conditions.”
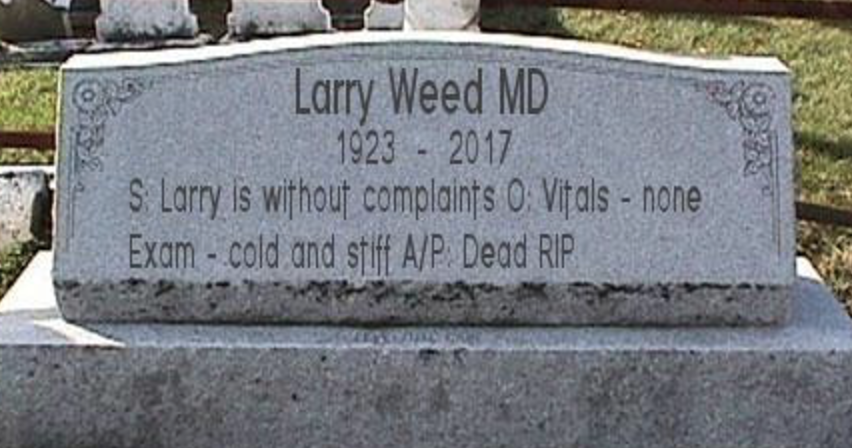
My late father, Dr. Lawrence L. Weed (LLW), made this point the day before he died. He was talking about the lost wealth of neglected patient data—readily available, richly detailed data that too often go unidentified and unexamined. Why does that happen, and what can be done about it?
The risk of missed information
From the very outset of medical problem-solving, LLW argued, patients and practitioners face greater risk of loss and harm than they may realize. The risk arises as soon as a patient starts an internet search about a medical problem, or as soon as a practitioner starts questioning the patient about the problem (whether diagnostic or therapeutic).
This gap creates high risk that information crucial to solving the patient’s problem will be missed. And whatever information the mind does deliver is not recorded and harvested in a manner that permits organized feedback and continuous improvement.Ideally, these initial inquiries would somehow take into account the entire universe of collectible patient data and vast medical knowledge about what the data mean. But such thoroughness is more than the human mind can deliver.
Guidance tools set standard of care
The only secure way to proceed, LLW concluded, is to begin investigation of medical problems (the “initial workup”) using guidance tools external to the mind. These tools must couple patient-specific data with general knowledge as follows:
- Link the initial data point (i.e., the patient’s presenting problem) with (1) medical knowledge about potentially relevant options and (2) readily available data for identifying those options (see the outer circle in the diagram below);
- Link the data in (2), once collected, with the knowledge in (1) to show how well the data match up with the combinations of data points defining each relevant option—this matching indicates which options are worth considering for the individual (see the middle circle in the diagram below); and
- Organize this information (data coupled with knowledge) into options and evidence—that is, diagnostic possibilities or therapeutic alternatives, the combined findings (positive, negative, or uncertain) on each alternative, and additional knowledge useful for assessing the best option to pursue (see the inner circle in the diagram below).
Tools to carry out these steps would define best practices and make them enforceable as high standards of care for the initial workup (i.e., patient history, physical exam, and basic lab tests). That threshold task is pivotal. It lays the informational foundation for follow-up thought and action by the patient and practitioner. That foundation is also needed for feedback activities to and from third parties. (See the diagram on p. 13 of Medicine in Denial.)
Patient-driven tools
In carrying out the initial workup, the patient’s role is always central. The tools should enable patients to enter history data, which is often the most detailed component of the initial workup. Moreover, the patient necessarily participates in the physical exam conducted by the practitioner, and reviews history, physical, and lab findings with the practitioner.
Tools for the initial workup must thus be used by patients and practitioners jointly. But patients must be able to initiate use of the tools unilaterally. They can’t rely on practitioners to recognize when serious medical investigation is needed. Patients are the ones who experience symptoms—who notice changes from what feels normal. To investigate whether these symptoms might be medically significant, patients need web-based tools for problem-specific inquiries. So do healthy persons who may simply require periodic screening checkups for unidentified problems (plus initial workup of any problems discovered).
Overcoming the medical Tower of Babel
Whether it is patients or practitioners seeking guidance for the initial workup, traditional medical practice leaves them both in a vacuum. Once that vacuum was filled solely by practitioners’ idiosyncratic judgments. Now the vacuum is also being filled with a plethora of practice guidelines and clinical decision support tools, not to mention internet search engine tools.
But the very multiplicity of all these resources defeats the purpose of defining generally accepted, enforceable best practices for initial workups. And the multiplicity is increasing with new patient-generated health data from sensors, wearables, and smartphone-connected devices for physical exam data. Moreover, the universe for needed guidance is expanding with vast new genomic/molecular data and knowledge.
The outcome of this multiplicity is not useful diversity but a Tower of Babel.
What we need instead are information tools with a unified design and trustworthy medical content, tools that guide users through the basic steps for inquiry into all medical problems, tools that take into account relevant information from all specialties without intellectual or financial biases. Users should not have to switch back and forth among different tools and interfaces for different medical problems, different specialties, different practice settings, different data types, different vendors, and different classes of users. The medical content captured in the tools must be problem-specific, but the tools’ basic design (see the three bullets above) should generalize to all problems in all contexts, as much as possible. This generality enables intuitive ease-of-use at the user level and powerful synergies at the software development level.
NLM’s role for the 21st century
LLW saw NLM as key to developing tools of this kind.
Drawing on its uniquely comprehensive electronic repository of medical content, NLM could create a new repository of distilled, structured knowledge. Drawing on its connections with the NIH research institutes and federal health agencies such as the CDC and FDA, NLM could rapidly incorporate new knowledge into that specialized repository. Outside parties and NLM itself could use that repository to build user-level tools with a unified design for conducting initial workups on specific medical problems.
This new infrastructure will encounter a barrier to its use—the medical practice status quo. Not all practitioners (or their overseers) will accept the data collection demands defined by the tool.By enabling creation of such a knowledge infrastructure for the public, NLM would seize an “opportunity to modernize the conceptualization of a ‘library.’” Beyond its current electronic repository, NLM could be “demonstrating how information and knowledge can best be developed, assimilated, organized, applied, and disseminated in the 21st century.” [NIH Advisory Committee to the Director, NLM Working Group, Final Report, p. 12 (June 11, 2015).]
Patients at the center
Here we return to the central role of patients.
Patients who unilaterally use NLM tools to complete the history portion of the initial workup can then seek out practitioners who are willing (and permitted) to use the same tools for the physical exam and basic lab test portions. By creating demand for those innovative practitioners and using the tools jointly with them, patients can drive medical practice toward a foundational reform.
Lincoln Weed, JD, Dr. Lawrence Weed’s son, practiced employee benefits law in Washington, DC for 26 years. He then joined a consulting firm where he specialized in health information privacy. He is now retired.